Cervical Dilation During Labour: Chart, Stages and Symptoms
Cervical dilation is a key aspect of the labour process, marking the body’s natural progression towards childbirth. During pregnancy, the cervix – the lower part of the uterus – remains closed to protect the growing baby. However, as labour begins, cervical dilation occurs, allowing the baby to move through the birth canal. Understanding the stages of cervical dilatation during labour, from initial contractions to full dilation, can help you know what to anticipate and prepare for the journey ahead.
What Does ‘Dilation’ Mean?
In the context of pregnancy, ‘dilation’ or ‘dilated’ refers to the opening of the cervix, a cylindrical, muscular organ at the lowermost part of the uterus that serves as a passage between the uterus and the vagina. During pregnancy, the cervix remains closed (0 centimetres dilated), firm and long, helping to keep your baby in the uterus until the right time for birth. So, if you’re 1 cm dilated, the cervix's opening is currently 1 cm wide.
What Is Cervical Dilation?
When labour begins, contractions help the cervix to soften and shorten, known as effacement, and finally open or ‘dilate’, allowing for the baby to travel from the uterus, through the birth canal, and out into the world. Cervical dilation is measured in centimetres, and for labour to progress effectively, the cervix needs to dilate from 0 to 10 centimetres, with 10 centimetres being the approximate width of a baby's head. This preparatory stage is an important part of the labour process.
When Do You Start Dilating?
The initiation of cervical dilation varies from person to person and pregnancy to pregnancy. Some pregnant people may begin to dilate weeks before they go into labour, while others may only start dilation after labour has begun. Here are some general timelines to help you understand how cervical dilation may play out in the final weeks of pregnancy and in the various stages of labour:
Keep in mind that each individual’s labour experience can differ. If you have any concerns about dilation or labour, speak with your midwife or doctor.
How Long Does Cervical Dilation Take?
Whether you’re 2, 3, 4, 5 or 10 cm dilated, you'll be eager to know how much longer it will be until you give birth. Though the amount of time cervical dilation takes can vary greatly among individuals, several hours are usually needed for the cervix to dilate from 0 centimetres (closed) to 10 centimetres (fully open). However, this can take longer if it’s your first pregnancy and may be quicker for subsequent pregnancies.
If it’s a first pregnancy, the latent (early) phase of labour can last anywhere from a few hours to a few days before labour becomes established. Once labour becomes established (the active phase), the process could last 8 to 18 hours. If you’ve given birth before, the process usually goes faster but can still last up to 10 or more hours.
Signs and Symptoms of Cervical Dilation
So, what does cervical dilation feel like, and what are the signs that you’re dilating? As your cervix begins to dilate during early labour, you may or may not experience some signs and symptoms. It’s uncommon to detect physical symptoms of your cervix opening; however, as labour begins, you’ll likely feel the uterine contractions that help dilation happen. Some other things you may notice as your cervix dilates are:
How Is Cervical Dilation Checked?
During labour, you may be offered a vaginal examination, performed by your midwife or doctor. They will generally use their fingers (gloved) to measure the width of the opening. It’s important to know that vaginal examinations are optional during labour, so it’s a good idea to discuss with your midwife whether you’d like them or not.
During your final month of pregnancy, your doctor or midwife may perform regular pelvic exams to check your cervix and see if there are any changes or signs of dilation. Once labour begins, they may continue to check your cervix every 4 to 6 hours to see how much it is dilating. Again, dilation of 10 centimetres is usually what a doctor or midwife is looking for in order to give the go-ahead to start pushing.
Self-checking your cervix for dilation at home is not recommended. It’s always best to leave this up to your midwife or doctor. So, if you suspect you’re in labour or labour is near, for example, you’re experiencing regular contractions or you’ve lost your mucus plug, contact your midwife.
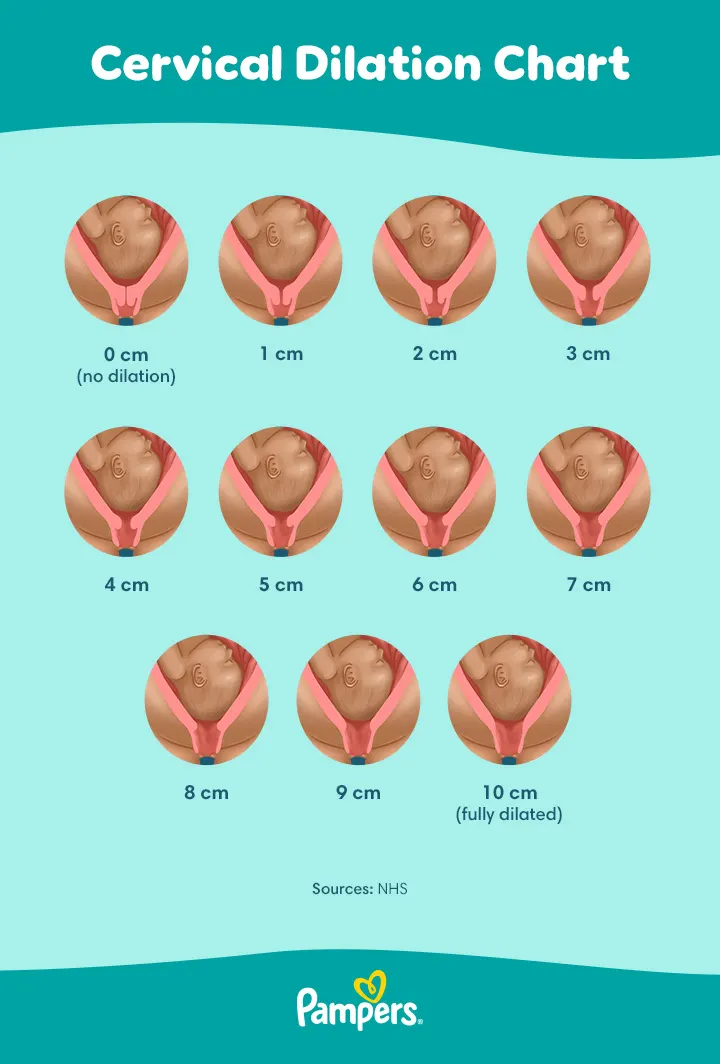
Cervical Dilation Chart
If you’d like a general idea of what a 1 cm dilated cervix looks like versus 3 cm, 5 cm or fully dilated at 10 cm, check out our dilation chart below.
How to Help the Dilation of Your Cervix
While cervical dilation is a natural process that cannot be rushed, there are some ways to help the body along if you’re wondering how to dilate the cervix naturally. During early labour, it may help to stay as relaxed as you can and alternate rest with activity. Some things to consider include:
Cervical Ripening
If your labour needs to be induced, your doctor or midwife may need to ensure your cervix is soft and thin, which is called ‘cervical ripening’, so that it will start to dilate during labour. Some methods your doctor may use to help your cervix dilate include:
Certain methods used to induce labour and start contractions may in turn help cervical dilation to progress. Among these methods are sweeping the amniotic membranes, administering oxytocin through an IV, and a procedure called an amniotomy (rupturing the amniotic sac).
When to Contact Your Doctor or Midwife
It’s essential to stay in close communication with your doctor or midwife throughout pregnancy, especially during the later stages. If you’re less than 37 weeks pregnant and experience any signs of premature labour, such as menstrual-like cramps, pressure in the pelvic area or lower abdomen or changes in your vaginal discharge, contact your doctor or midwife immediately. They will likely do a pelvic exam to look for any cervical changes or dilation and monitor your contractions.
If you’re 37 weeks or more, keep an eye out for signs of labour and contact your midwife when you start experiencing any. They can tell you what the next step is and when you need to go to the hospital.
FAQS AT A GLANCE
Cervical dilation refers to the size of the opening in the cervix. During labour, the cervix opens from being closed (0 centimetres) to fully open (10 centimetres), allowing the baby to pass through the birth canal.
The Bottom Line
Cervical dilation is a natural and necessary part of the labour and vaginal delivery process. By understanding the process of dilation, and the signs and symptoms, you can approach your birth experience with confidence. Remember to stay in touch with your healthcare team and trust in your body's ability to progress at its own pace.
Read more about Pregnancy
Join Pampers Club and get: