Mastitis Symptoms and Treatment
Key Takeaways
Mastitis is an inflammation of breast tissue that may result from a blocked milk duct, a bacterial infection or a combination of the two, causing hotness, tenderness and pain in one (or more rarely both) of your breasts.
Having mastitis can be very frustrating, especially if you are breastfeeding, but it is treatable if you recognise the early signs and take steps to alleviate it.
Read on to find out what causes mastitis, and how you can prevent mastitis or treat the symptoms so you can get back to breastfeeding your little one without discomfort as soon as possible.
What Is Mastitis?
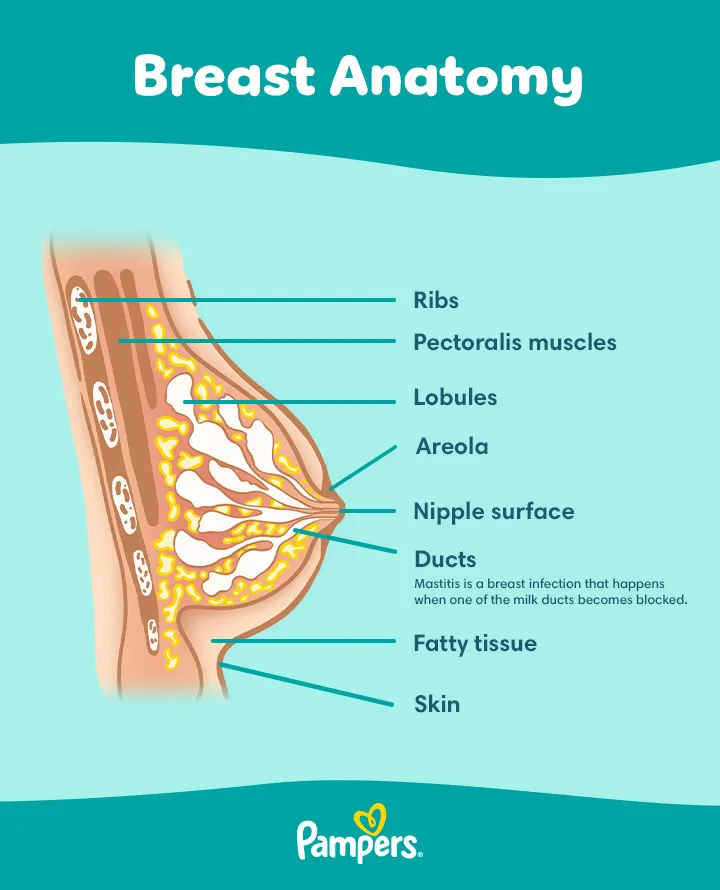
Mastitis is an inflammation of the breast that can sometimes be caused by a build-up of milk causing a milk duct in your breast to get blocked.
When this happens, your body reacts in the same way as it would to an infection: by sending more blood to the affected area. This is what causes the redness, tenderness and swelling associated with mastitis.
With mastitis a hard lump can form, and your breast can become tender and sore. If the clogged duct isn’t cleared quickly, a breast infection may set in.
Mastitis is most common in breastfeeding mums and mums who are expressing their milk, but it can also happen in people who aren’t producing breast milk — sometimes even men get it.
The mastitis that’s related to breastfeeding or expressing milk is referred to as lactational mastitis. This article will focus on this kind of mastitis.
Mastitis Symptoms
You may be wondering how to tell the difference between mastitis and the normal tenderness you might feel when you first start breastfeeding.
The symptoms of mastitis often appear suddenly, and usually affect only one breast. These symptoms can include
What Causes Mastitis
Lactational mastitis – that is, mastitis related to breastfeeding or expressing milk – is most likely to occur if your breasts don’t empty completely during feeds. This can cause milk to build up and become trapped in the milk ducts.
Mastitis can also result from a bacterial infection, or an infection may develop as a result of mastitis that starts out with a blocked milk duct. Here are some things that might increase your risk of developing mastitis:
Treatment for Mastitis
Although mastitis can be uncomfortable or painful, the good news is it’s usually easy to treat and soon clears up, especially if you catch it early.
If the mastitis doesn’t start clearing up within 24 hours with the home remedies described below, your doctor may prescribe antibiotics that are safe for your baby too, should you be breastfeeding your little one.
Self-help Methods to Relieve Mastitis Symptoms
If you start experiencing the early signs of mastitis, you might try some of these self-help methods to ease the discomfort:
Antibiotics
If the symptoms of mastitis don’t start easing up within 24 hours, or if there’s any other reason to suspect a bacterial infection in your breast, your doctor will likely prescribe a course of antibiotics.
Always follow your doctor’s instructions on how to take any medicines that are prescribed for you. If the symptoms don’t start getting better within 48 hours after starting to take antibiotics, it’s a good idea to go back to your doctor.
When to See the Doctor
Early treatment of mastitis is important. See your doctor if the symptoms get worse or don’t clear up within 24 hours despite trying some of the self-help methods mentioned above. If it’s left untreated, mastitis can develop into a painful breast abscess, which may need hospital treatment.
If you are considering taking a painkiller, always ask your doctor or health visitor first which pain relief medication may be safe to take while breastfeeding.
Check in with your doctor straight away if you have any other symptoms – such as a fever, aches or chills, or if you’re at all concerned about what you’re experiencing.
In very rare cases, mastitis can develop into sepsis, which needs urgent medical attention. Call an ambulance or go to your local A&E unit if you have mastitis and experience dizziness, slurred speech, confusion, nausea, vomiting or diarrhoea.
Can You Keep on Breastfeeding With Mastitis?
Yes you can. In fact, sticking to your regular feeding routine is usually the best thing you can do if you have mastitis. Keeping up a steady flow of milk helps to clear any blockages in the milk ducts.
That’s not all: If you stop breastfeeding, it could actually make the symptoms worse as your breasts continue to produce more milk that has nowhere to go.
Rarely, you might find that the mastitis makes feeding from the affected breast too painful. If that’s the case, it might help to gently express a little milk from the affected breast and either store it for later or feed it to your baby straight away using a bottle.
After relieving some of the pressure in this way, you might be able to finish nursing on the affected breast without too much discomfort.
Does Mastitis Affect Breast Milk?
Breastfeeding while you have mastitis won’t harm your baby. Even if you have an infection, it won’t be passed on. If you’re taking antibiotics for your mastitis this doesn’t present a risk for your little one either, as long as your doctor knows that you’re breastfeeding you’ll be prescribed a medicine that is safe to take.
Keep in mind, a tiny amount of the antibiotics may be passed into your breast milk and this could make your little one a little irritable, and his or her poo may be a bit runnier while you’re taking them.
How to Prevent Mastitis
Here are some things you might like to try to help prevent mastitis in the first place:
FREQUENTLY ASKED QUESTIONS
Breastfeeding or expressing with mastitis can be difficult and frustrating. Try to be patient and gentle with yourself during this time.
Keep in mind that continuing to breastfeed will speed up recovery and help stop the mastitis from worsening, and you’ll keep giving your baby the benefits of your breast milk, such as extra protection from infections and diseases.
As long as you recognise the early signs of mastitis and see your doctor as soon as possible if necessary, it won't be long until you're back to enjoying this bonding time with your baby.
How we wrote this article
The information in this article is based on the expert advice found in trusted medical and government sources, such as the National Health Service (NHS). The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
Read more about Newborn Baby
Join Pampers Club and get: