Bedwetting (Nocturnal Enuresis) in Children
Bedwetting in children might be more common than you think. Known medically as nocturnal enuresis, most children outgrow this type of bedwetting by 5 years old, but for some, it may still continue. Although bedwetting can be challenging for you and embarrassing for your child, there’s plenty you can do to help your little one through this common phase.
What Is Bedwetting (Nocturnal Enuresis)?
When wetting the bed happens in children only during sleep, it’s officially called night-time incontinence or nocturnal enuresis, or, more commonly, bedwetting. This involuntary urination happens while your child is asleep and is fairly common, affecting about half a million children in the United Kingdom.
A familiar morning scene in many households may include wet sheets and pyjamas, and an embarrassed child. But know that this doesn’t mean your efforts with potty training have gone down the drain! This is a normal part of your child’s development and there are many bedwetting solutions that you can try.
How Common Is Bedwetting in Children?
All children wet the bed and have ‘accidents’ at some point during the long task of potty training. This is a normal, expected part of the learning process! Bedwetting will undoubtedly occur as your child starts potty training, which usually takes place between the ages of 2 and 3 years.
As your little one works their way through potty training, bedwetting gradually becomes less prevalent and eventually disappears altogether. In many children, this happens around the age of 5, but it’s still normal for your child to wet the bed after turning 5. Staying completely dry at night is the final leg of the potty-training process, and some children take longer than others to complete it.
Keep in mind that bedwetting still happens in 20 percent of 5-year-olds, six percent of 7-year-olds and in over one percent of teenagers. Additionally, bedwetting runs in families as follows:
If one parent wet the bed as a child, your little one has a 40 percent chance of doing the same.
That chance increases to 70 percent if both parents wet the bed.
Therefore, bedwetting (nocturnal enuresis) in children is quite common and isn’t anyone’s fault – certainly not the fault of your child.
What Causes Bedwetting?
Not long ago, medical experts considered bedwetting a simple issue that children would eventually outgrow without treatment or help. Today, it’s better understood as a more complex issue involving several factors.
Thanks to this understanding, we now know that there are four main reasons why bedwetting happens in children:
Children’s bladders can’t stretch enough to make room for all the wee they produce while sleeping
Children tend to produce more wee at night – too much for their bladders to handle even if the bladder did properly stretch
Although the bladder may send a signal that it’s full, children don’t tend to wake up from it
Children may wet the bed when feeling stressed or emotional about situations at home or school.
In addition to these common causes of nocturnal enuresis in children, there are a few potential underlying health issues that can influence your little one to wet the bed:
Constipation. If your child is dealing with constipation, the hard poos in the bowels could press against the bladder, prompting it to empty at night.
Urinary tract infection (UTI). Daytime bladder issues like a UTI can also contribute to nocturnal enuresis. If your child also has a fever or pain while weeing, contact the doctor.
Type 1 diabetes. One of the symptoms of type 1 diabetes is excessive urination, which could also occur at night. Consult your GP if your child also appears thirstier or more tired than usual and/or if they’ve lost weight.
In Summary There are four main reasons why children wet the bed: a too-full bladder; a bladder that can’t stretch enough to hold the wee produced at night; not waking when the bladder sends a signal that it’s full; feeling stress at home or school. Additionally, if your child has any of the following underlying health conditions, they might face bedwetting more often: constipation, urinary tract infections (UTIs) and type 1 diabetes. |
Solutions for How to Manage Bedwetting
Although the ‘watch and wait’ tactic was once the go-to solution for bedwetting – as experts believed children would eventually outgrow the behaviour – this method is no longer recommended. If left untreated, children might not outgrow bedwetting, and research shows that the sooner you address bedwetting, the sooner your little one may have dry nights.
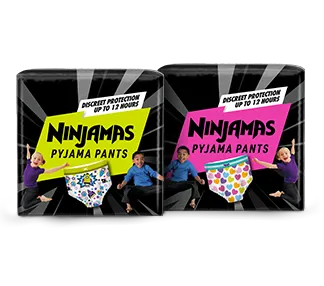
It takes time and patience, but you’ll get there in the end! In addition to the 10 tips below, wearing Ninjamas Pyjama Pants to bed can ease anxiety and help your child wake up confident by keeping their skin (and bedclothes) dry and comfy through the night. Ninjamas come in 2 sizes: 4-7 years and 8-12 years. The cool designs, a choice of colours and Quietcloth material mean they don’t look, feel or sound like nappies – so older kids can wear them with confidence too.
Here are 10 tips for how to manage bedwetting in children:
Don’t punish or blame children for bedwetting and stay positive and encouraging
Help your child feel less embarrassed or ashamed after the incident by reassuring them that accidents happen. Explain that bedwetting isn’t their fault, that it happens to many children and with some effort and patience, it usually goes away in time
If bedwetting runs in the family (for example, if a parent was a bedwetter), make your child aware so the situation feels more relatable
Because constipation can be an underlying cause of bedwetting, provide your child with lots of cereals, fresh fruit and vegetables
Track your child’s bedwetting patterns in a nightly diary to help you and your doctor better understand why bedwetting is happening, how treatment is working, or if any is needed
Ask your child to help change the sheets after a bedwetting incident and reward them for their help (rather than rewarding them for a dry bed in the morning, as that’s out of their control)
Pay attention to your child’s urine and bowel movements throughout the day. Although everyone is different, it’s typical for children use the potty or toilet four to seven times a day, pooing at least four times a week. Going less than that could indicate a bladder issue or constipation, which may contribute to nocturnal enuresis
Encourage your child to use the toilet before going to bed; and, although it’s important to drink plenty of liquids during the day (six to eight glasses of water), have them stop drinking about one hour before bedtime
Set up your child for success by providing them with a nightlight and moving them from the top to lower bunk (if applicable) so it’s easier to use the loo at night
Although there aren’t many psychological causes of bedwetting, children may wet the bed when feeling stressed or emotional, such as about something at home or school.
In Summary The key to managing bedwetting in children is not to scold them or make them feel ashamed. Instead, remain calm and help them understand that it was an accident, it happens to many children and, with effort, it will go away in time. To manage your child’s nocturnal enuresis, pay attention to their urine and bowel movements during the day, encourage using the potty before bedtime, provide a diet of fibrous foods like fruits and vegetables and use a plastic mattress cover, among other things. |
When to See the Doctor About Bedwetting
Bedwetting is not usually a cause for concern, even after potty training. However, experts recommend that children who are still not dry at night by the age of 5 see their doctor to help identify the causes.
Many communities and schools offer specialised healthcare professionals and clinics for enuresis. Because the causes of bedwetting can be complex, the doctor will first determine why your child is still experiencing nocturnal enuresis before suggesting a solution.
Your doctor is also available to help when
You’ve tried all the advice from above and your child still wets the bed
Your little one starts wetting the bed after they’ve been dry for more than six months.
Regardless of what stage you’re at with potty training and bedwetting, your doctor is always there to help! Consult your GP if you and your child are finding it difficult to manage bedwetting for any reason.
Solutions for Bedwetting (Nocturnal Enuresis)
In some cases, the doctor may recommend simple home treatments for your child, such as discouraging them from drinking liquid before bedtime. If constipation or diabetes is an issue, the provider may recommend treatment for that. However, there are also other methods the doctor might suggest you try, such as using medication or a bedwetting alarm.
Bedwetting Alarm
Bedwetting alarms are often the first solution recommended for kids and teenagers under the age of 19. They’re effective in that they train children to wake up when they need to wee.
The bedwetting alarm works by awakening your child as soon as it senses wetness. However, the device isn’t fool proof. Many children sleep right through the alarm! You, as the parent, may need to step in and wake up your child when you hear the alarm.
When used according to the doctor’s instructions, a bedwetting alarm may help condition your child to wake up when they need to use the potty. Try to be patient, though, as it may take at least four weeks of use to be successful.
Medication
Oral medicines prescribed by the doctor are also a possibility for older children. They work by prompting the kidneys to produce less wee, so your child should take the medicine right before going to bed. These types of medications may come in handy when used occasionally for specific situations, such as sleepovers and summer camp.
If your little one is still bedwetting after trying these solutions, the doctor might recommend other forms of medication or treatment on a case-by-case basis.
In Summary If your child is still experiencing bedwetting after the age of 5, it’s best to consult a doctor or nurse at an enuresis clinic for guidance. The doctor may want to run some tests to rule out a medical condition and, depending on your child’s age, recommend solutions like using a bedwetting alarm or prescription medication. |
FAQS AT A GLANCE
Bedwetting has four typical causes in children:
- A too-full bladder
- A bladder that can’t stretch enough
- Not waking when the bladder sends a signal that it’s full
- Feeling stressed at home or school.
The Bottom Line
Bedwetting has happened to just about everyone – possibly even you when you were a child! It isn’t uncommon for children to experience bedwetting during daytime and night-time potty training. And although most children outgrow bedwetting around the age of 5, for some, nocturnal enuresis may continue.
There are many reasons your child might wet the bed, and none of them are your little one’s fault. So, try to stay positive and always reassure your child that it was just an accident and that it happens to many children. Meanwhile, there’s plenty you can do to manage the bedwetting, such as encouraging your child to use the loo before going to sleep, and to drink enough in the daytime so there’s no need for a bedtime drink.
If you’re concerned about your child’s bedwetting or your little one is still wetting the bed after turning 5 years old, see a doctor for guidance. The doctor may recommend the use of a bedwetting alarm to help condition your child to wake when they need to wee or may decide to prescribe medicine. In rarer cases, tests may indicate that the bedwetting is due to a medical condition that needs to be treated.
Rest assured that sooner or later – with a little bit of patience, effort and encouragement – every child, including yours, will outgrow bedwetting.
The information in this article is based on the expert advice found in trusted medical and government sources, such as the National Health Service (NHS).The content on this page should not replace professional medical advice. Always consult medical professionals for full diagnosis and treatment.
Join Pampers Club and get: